Traumatic Brain Injury
Women May Have Worse Outcomes After a Brain Injury Than Men
And they may be at greater risk for dementia. Here's why.
Posted February 24, 2023 Reviewed by Davia Sills
Key points
- Women tend to experience worse cognitive and psychological outcomes after a traumatic brain injury than men do.
- Because clinical treatments have been predominantly tested on men, current treatments may not be as effective for women.
- Changes in sex hormones across a woman’s lifespan play a key role in why sex differences occur in outcomes and treatment response.
Traumatic brain injury (TBI) is a major cause of disability and death in the U.S., leading to over 223,000 hospitalizations in 2019 and over 64,000 deaths in 2020. Recent findings indicate that your sex may impact the effects of TBI on cognitive function and responsiveness to treatment. Unfortunately, some of these sex differences increase women's risk for dementia.
What does TBI do to the brain?
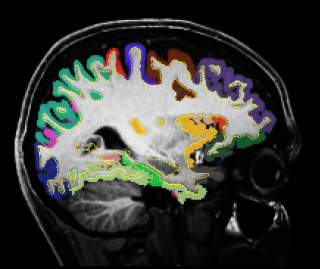
TBI often is caused by a blow or bump to the head, for example, from falling down the stairs, or from a car accident. Generally speaking, TBIs damage the white matter in the brain, which is important for communication between different brain parts. TBIs also can lead to loss of consciousness, hematomas (pooling of blood in the brain tissue), brain swelling, and skull fractures. Symptoms vary depending on which brain area was affected, as well as the severity of the TBI. Fortunately, 80 percent of reported TBIs are considered to be of mild severity.
Differences in outcomes
Many studies show that women have poorer outcomes than men, such as experiencing more severe or more frequent headaches, depression, short-term memory complaints, sleep problems, and anxiety than men. Dr. Maheen Adamson, Director of Research at the VA national Women’s Operational Military Exposure Network (WOMEN) and professor of neurosurgery at Stanford, is one of the foremost scientists studying how and why female veterans' experience of TBI differs from that of male veterans. She and her team have found that among female and male veterans with TBI, women experienced more psychiatric problems and more vertigo, and even though they tended to have more years of education than male veterans, they were more likely to be unemployed and to be living alone.
In the first study to closely match female and male veterans on key variables such as the severity of TBI, years since TBI, and current age, Dr. Adamson's team found that female veterans had substantial decreases in cortical thickness, which was then correlated with poorer performance on some cognitive tests. Male veterans, on the other hand, showed negligible reductions in cortical thickness. Other studies also have found that decreased cortical thickness is associated with impaired cognitive function and increased risk for dementia.
Due to a confluence of factors, women with TBI may have a higher risk for dementia. First, TBI increases the risk of dementia even when a TBI occurred over 30 years ago. The greater cognitive impairment and reduced cortical thickness that some women experience after a TBI may increase this risk even more. Second, women frequently report experiencing depression after TBI; depression increases the odds of dementia by 1.5 to 2.6 times. Given that age is the biggest risk factor for dementia, the probability of dementia among older women with TBIs may be even greater.
Dr. Adamson worries about the effect of TBI on women veterans' dementia risk. "Cognitive impairment and dementia are also devastating outcomes of TBI. A history of moderate TBI confers a greater than twofold risk of developing Alzheimer's disease." The significant increase in the active-duty female military in recent years is likely to correspond with a proliferation of female combat-related injuries. Her findings "outline a perfect storm of physical brain injury, depression, and astounding financial, psychological, and societal impacts that will lead to a tsunami of dementia among women veterans."
Differences in treatment response
Because TBI symptoms can vary widely from one person to the next, a personalized combination of treatments is typically prescribed. Treatments can include medication, surgery, and rehabilitation. Dr. Adamson's group uses neuromodulation to improve cognitive function, in which nerve cells in the brain are stimulated. She finds that women tend to need more sessions of neuromodulation than men to achieve similar levels of improvement.
This finding may stem from men being overrepresented in clinical studies assessing the utility of these treatments. One review paper found that 80 percent of clinical studies for a particular type of neuromodulation called transcranial magnetic stimulation only included male participants. As Dr. Adamson put it, "if you start with methods that are developed on men, they are going to work better in men."
Why are there sex differences with TBI?
Dr. Helen Bramlett, Professor of Neurological Surgery at the University of Miami Miller School of Medicine, thinks that "hormone fluctuation is one of the root causes" for sex differences in TBI outcomes. She and her colleagues recently wrote a comprehensive review article that described how TBI might impact women differently at each life stage due to the presence or absence of hormones. "You can divide the female lifespan into several very distinct parts based on the fluctuation of hormones or the level of hormones at a particular stage. The levels of hormones change as one moves from adolescence to pregnancy, in some cases, post-pregnancy, perimenopause, menopause, and post-menopause. The levels of hormones that are present during a TBI may influence how well a person does after the TBI." For example, women who have recently completed menopause, who typically are in their 50s, have significantly better outcomes after TBI than women in the perimenopause stage, who tend to be in their 40s.
What women should do after experiencing a TBI
To reduce the impact on dementia risk, Dr. Adamson recommends lifestyle activities, such as regular exercise, a healthy diet, and stress management. Because there has been a male bias in the clinical treatments developed so far, she also recommends "asking your doctor if their recommended treatment has been demonstrated to be effective for women."
Summary
Women's experience of TBI, from outcome to treatment responsiveness, is distinct from that of men and may increase their risk for dementia. While the underrepresentation of women in TBI studies, particularly in clinical trials, is dispiriting, Dr. Bramlett remains optimistic, "I do think there's become more awareness in needing to make sure that the research you are conducting covers both males and females. If you don't, you're not only doing a disservice to women but to yourself as a scientist."
References
Resources
A fantastic resource for women who’ve experienced TBIs or professionals who want to learn more is the PINK Concussions group. As explained by Katherine Snedaker, LCSW, the CEO and Founder of the organization, “Each year, PINK Concussions presents over 50 hours of trainings for the public, civilian and military medical professionals on the sex and gender differences in brain injury, publishes original research on this topic, and moderates support groups for over 8,000 members available 24/7.” Female veterans can participate in the VA Women’s’ Health Research Network, which aims to increase evidence-based health care for female veterans by supporting VA researchers in conducting female veteran health research.
Adamson, M, Main, K., Harris, O., & Kang, X. (2021). Sex differences in cortical thickness and diffusion properties in patients with traumatic brain injury: A pilot study. Brain Injury, 36:4, 488-502.
Blaya, M. O., Raval, A. P., & Bramlett, H. M. (2022). Traumatic brain injury in women across lifespan. Neurobiology of disease, 164, 105613.
Centers for Disease Control and Prevention. Traumatic Brain Injury and Concussion. Retrieved from https://www.cdc.gov/traumaticbraininjury/data/index.html
Gupte R, Brooks W, Vukas R, Pierce J, Harris J. (2019). Sex Differences in Traumatic Brain Injury: What We Know and What We Should Know. Journal of Neurotrauma. 36(22):3063-3091
Lippa SM, Brickell TA, Bailie JM, French LM, Kennedy JE, Lange RT. (2018). Postconcussion Symptom Reporting After Mild Traumatic Brain Injury in Female Service Members: Impact of Gender, Posttraumatic Stress Disorder, Severity of Injury, and Associated Bodily Injuries. Journal of Head Trauma Rehabilitation 33(2):101-112.
Lutkenhoff ES, Wright MJ, Shrestha V, Real C, McArthur DL, Buitrago-Blanco M, Vespa PM, Monti MM. (2020). The subcortical basis of outcome and cognitive impairment in TBI: A longitudinal cohort study. Neurology. 95(17):e2398-e2408.
Munivenkatappa A, Agrawal A, Shukla DP, Kumaraswamy D, Devi BI. (2016). Traumatic brain injury: Does gender influence outcomes? International Journal of Critical Illness and Injury Science. 6(2):70-73.
National Institute of Neurological Disorders and Stroke. How does TBI affect the brain? Retrieved from https://www.brainline.org/article/how-does-tbi-affect-brain
Nordström A, Nordström P. (2018). Traumatic brain injury and the risk of dementia diagnosis: A nationwide cohort study. PLoS Medicine. 15(1):e1002496.
Pettigrew C, Soldan A, Zhu Y, Wang MC, Moghekar A, Brown T, Miller M, Albert M; BIOCARD Research Team. (2016). Cortical thickness in relation to clinical symptom onset in preclinical AD. Neuroimage: Clinical. 12:116-22.
Phillips, A., Sami, S., Adamson, M. (2020). Sex Differences in Neuromodulation Treatment Approaches for Traumatic Brain Injury: A Scoping Review. Journal of Head Trauma Rehabilitation 35(6) 412-429.
Yang, W, Li, X, Pan, K-Y et al. (2021). Association of life-course depression with the risk of dementia in late life: A nationwide twin study. Alzheimer's and Dementia. 17: 1383– 1390.




