Health
How to Access Therapy for Your Child
A parent consultation and your involvement improves child mental health, too.
Posted December 7, 2021 Reviewed by Ekua Hagan
Key points
- Since COVID-19, mental health difficulties in children have increased 35% in the UK, and there is a shortage of child psychologists.
- Instead of face-to-face therapy for a child, which can be hard to access, indirect Parent Consultations are effective and have many benefits.
- An increase in Parent Consultations could significantly reduce wait times for children to be seen directly for talking therapy.
In the UK, many child psychologists and child therapists are at capacity and there is a shortage of trained professionals. The average published waiting time is more than six months for treatment of children with mental health difficulties on the National Health Service (NHS); but from my own recent professional experience, the wait time can be up to two years.
Since COVID-19, mental health difficulties in children in the UK have seen an increase of 35%, increasing from 1 in 9 children to 1 in 6 (Lennon, 2021). There is restricted access to face-to-face talking therapy, with a boom in online therapy solutions. Parents and children, though, often prefer face-to-face therapy, and younger children, or those living with disabilities, are much more likely to engage in face-to-face therapy. (In this post, “parents” can mean any adult, step-parent, family member, foster carer, or caregiver with responsibility for the child).
Parent Consultations
So, what can psychologists, counsellors, and psychotherapists offer that is effective in treating a child’s symptoms indirectly instead, particularly online? Parent Consultation is one answer. (For deeper insights into different cultural models, definitions, and theories behind Parent Consultations see Holcomb-McCoy, 2009.)
For small children, and those displaying behavioural issues, psychological interventions are often more effective through the parents, carers, or adults in the system, environment, or context. Modern psychotherapy is based on the Freudian adult model of the psychotherapist talking to the client on the couch for 50 minutes, and this has left us with a lasting bias toward how therapy should be delivered. This one-to-one model does not readily take into account how children learn, develop, relate to others, communicate, or perceive the world.
Taking Part in a Parent Consultation
So, what does a Parent Consultation entail? Is it like the parent going to therapy instead? What if you really feel that the child needs the therapy and not you? And what if you simply cannot find more time to go to yet another appointment, when you have more than one child, a job, other caring roles, and you feel overwhelmed?
Parent Consultations need not be stressful interventions. Often, sessions can be brief, supportive, solution-focused, and time-limited. There can be whole-family benefits. I’ve seen in my practice that, often, even a single Parent Consultation can be effective. Sommers-Flanagan (2007) shows that parents reported being less stressed and more capable of managing behaviour that challenged others following a single-session consultation. The space is also confidential and private (unless there are risks that require breaches of confidentiality by law).
A trained therapist will approach you with a warm, open, non-judgmental, and curious perspective, just like a therapy session. You will be the expert on your lives and the therapist can bring his/her skills, years of clinical practice, research, and training to come up with a shared understanding, or “formulation” of the problem and your goals. You can then take this awareness and clarity forward into your daily lives to make some improvements for your child and family. Figure 1 shows some main topics in Parent Consultations.
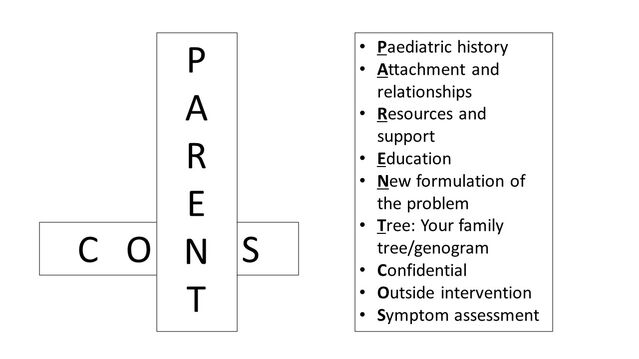
Consultations can also include education about the psychological condition (psychoeducation):
- Paediatric history: This includes pregnancy, birth, the child’s milestones, and development and health issues.
- Attachment: Assessment of attachment/relationship with significant caregivers and siblings.
- Resources: Mapping out a system of resources and support.
- Education: How your child is doing at school.
- New Formulation: A new psychological formulation of the problems using the child’s history and symptoms combined with psychological research and evidence. It can be a relief to see a new understanding emerging rather than being stuck with the problem-saturated story. Formulations are usually more helpful if they include the child and family’s strengths, not only the difficulties.
- Tree: Mapping out a family genogram (family tree) or transgenerational patterns; family beliefs, culture, religion, heritage, ethnicities.
- Confidential: It is a confidential space to voice concerns about your child and talk about dynamics at home, school, or university.
- Outside Intervention: Parents, teachers, and adults in the system can play a part in evidence-based interventions outside the therapy sessions i.e. at home or in school.
- Symptoms and Behaviour: An understanding of your child’s symptoms and behaviour—what you are seeing.
Child-Parent Well-Being Cycle
From my experience, many young people speak with compassion about their parents and try to see and appreciate all they are doing for them. Of note is that, often, children come with concerns for the parent and concerns about not wanting to burden them further. Parental anxiety can impact the child’s levels of anxiety. You might find you have your own stressors and concerns and might need your own support, childcare, resources for work, or help with your relationships. Our children and adolescents pick up on if caregivers are not physically or mentally well and, without the right tools, support, or coping strategies in place for you, this could impact them.
The issue is that the parents could benefit from having a psychologically informed perspective on where their child is coming from, their world, and their pressures. With this knowledge, parents are more likely to feel empowered and work together with their children, and the system around them, to make positive changes.
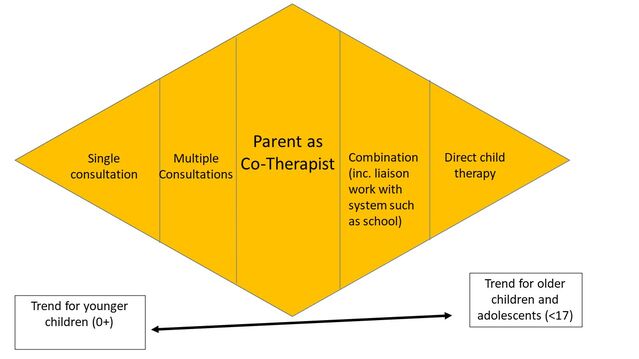
Degrees of Parental Involvement in Therapy
Figure 2 shows some of the different ways parents can contribute meaningfully to their child’s therapy by being involved by different degrees. I find that younger children tend to benefit from single-parent consultations with children with more verbal, reflective, and self-reflective skills benefitting from direct therapy. This is a model to outline our own practice at Lifespan Psychology; further research would be necessary to test the model.
Below I describe several composite case studies in which aspects of different families’ stories are taken from my clinical practice and blended in order to create one meaningful fictional child and family.
Parents as Co-Therapists
For an 11-year-old boy who had recently suffered a bereavement, his way of coping was sleeping in his parents’ bed. The problem was getting worse over time because he could not sleep alone at all and would wait for both parents to go to bed. Using a “fear ladder” (graded hierarchy) with rewards at each step; using soft toys for comfort and rewards, and gradually reducing the number of hours in his parents’ bed, we were able to encourage parents to empower the child to sleep alone over a period of six weeks. The child was able to focus on other things that gave him security such as making new friends and collectively this contributed to higher self-esteem.
Single Parents’ Consultations
With a 13-year-old girl who was wetting the bed, Dad and I had a consultation which included how frightened she was after his stroke. She was frightened of it happening again. The bed-wetting ended when Dad was able to reflect on how worried his daughter was about his health. He made a conscious effort to lower his stress levels, particularly around her, so she would worry less about his health. Parents were also advised to ask the daughter to help with the laundry so Mum did not always have to do it, and this consequence also seemed to help motivate her. The bed-wetting stopped within one month.
Multiple Parents’ Consultations
For a 14-year-old boy with OCD contamination fears and handwashing until his hands were bleeding and sore, Mum and Dad were invited to complete a Family Accommodation Scale. The scale showed that Dad was helping his son by opening doors he would not touch and turning on taps for him. Gently encouraging Dad to withdraw from routines using praise and reward gradually helped his son to stop being afraid, specifically, that not washing his hands every 30 minutes would lead to the death of his family. Within 10 weeks, the obsessive thoughts about contamination became less frequent.
Combination/System Working
A 5-year-old child with encopresis (soiling) for one year at school was able to overcome this in sessions, by making going to the toilet fun. We created a narrative storybook of cartoon characters coming to put the “poos down the loo” at school. Teachers’ involvement at school, and parents mirroring these interventions at home, led to a successful intervention within eight weeks.
Direct Child Talking Therapy
Engaging a child of any age in sessions can be creative and rewarding when using different tools and multimedia. I use cognitive behavioural therapy (CBT), a systemic, narrative, and behavioural therapy, as well as integrative therapy, which is a combination of different therapies. Some children may prefer shorter sessions or involve a game, activity, or parental involvement.
National Recommendations
I predict that if Parent Consultations were rolled out nationally, there could be a significant reduction in the waiting times for children to be seen directly for talking therapy. NHS England /UK, and private medical insurance companies, could consider this as an option for children and families waiting for treatment, as their frameworks for funding are often focused on direct contact with the client—in this case, the child.
As parents and carers, it is usually us who spend the most time with our children. We realise how deeply embedded in our contexts we are as adults, and how our contexts and environments impact our overall well-being. You could argue that children’s outcomes are context-dependent even more so than adults', due to their level of need and dependence on adults. Parent Consultations offer an opportunity for parents to gain knowledge and intervene within the child’s context to make a significant impact on their mental, emotional, social, educational outcomes and well-being. This is likely to have a reciprocal, positive effect on us as parents, and the family overall.
To find a therapist, please visit the Psychology Today Therapy Directory.
References
Lennon, M. (2021). The State of Children’s Mental Health Services 2020/21. Children’s Commissioner for England.
Holcomb-McCoy, C. (2009). Cultural Considerations in Parent Consultation. Professional Counseling Digest, APA.
Sommers-Flanagan, J. (2007). Single-Session Consultations for Parents: A Preliminary Investigation. The Family Journal: Counselling and Therapy for Couples and Families.
I discuss this in greater detail on my latest guest appearance on the podcast Episode 70: "The Gift of Knowing How to Support Your Child With Their Mental Health | Wisdom for Working Mums."




