Estrogen
Changes in Estrogen Impact the Brain Well Before Alzheimer's
Could hormone change around menopause be a starting point for the disease?
Posted April 4, 2022 Reviewed by Davia Sills
Key points
- Alzheimer's disease has become a growing problem now that people are living longer, and women are at a particularly high risk.
- The changes in estrogen production that occur from menopause on may play a role in whether a woman develops Alzheimer's or not.
- Taking steps to address hormonal imbalances sooner rather than later may reduce the risk of Alzheimer's.
Aging is a natural process of mental and physical change. During adolescence, for example, the accelerated development of the body coincides with the psychological stress and volatility of the developing mind. Later in life, passage into old age (classified as 65+) often involves physical and, to varying degrees, cognitive decline. Yet adolescence is a gateway to adulthood, and with age comes the benefit of knowledge and framing perspective.
In much of the world today, humans can expect to live into old age. In the United States, the average lifespan is now about 80 years for a woman and 75 for a man. It is astonishing to consider that life expectancy has practically doubled since the turn of the 20th century, when the average life expectancy was 48 for women and 46 for men.
Living longer, however, also comes at a price for both the individual and society. Public health care costs and the familial burden for the care of the aging population have grown exponentially during the past few generations. Along with heart disease and cancer, Alzheimer’s is now one of the top six leading causes of death in individuals over 65.
Unlike natural brain aging, which proceeds gradually and with a slow loss in some brain function, the common form of Alzheimer’s (sporadic) is a devastating illness with unknown causes. The disease strikes in connection with an accumulation of tau and amyloid-type proteins in the brain, yet why and how protein buildups occur is not understood. Their presence appears to set the stage for a destructive form of brain inflammation and a cascade of molecular events that leads to physical and mental deterioration. Brain regions important for memory storage and language processing are especially at risk, which explains the hallmark symptoms of the disease.
Old age is the greatest risk for developing Alzheimer’s, but being a woman is the second-highest risk factor. Women make up two-thirds of all disease cases, and after the age of 60, a woman’s chance of developing Alzheimer’s becomes twice that of a man. Why women are at such heightened risk is not clear, but evidence suggests a link between the decline in estrogen production around menopause and the health of the aging brain.
Scientists still don’t understand exactly how a drop in circulating estrogen can predispose women to Alzheimer’s disease, especially since it is hard to know when the disease begins. In most cases, by the time symptoms arise, neural damage appears to have already occurred. Some experts propose that the start of the disease may occur years, if not a decade, before any cognitive and behavioral signs. Important changes in brain hormone signaling around menopause may provide a critical point for progressive brain damage.
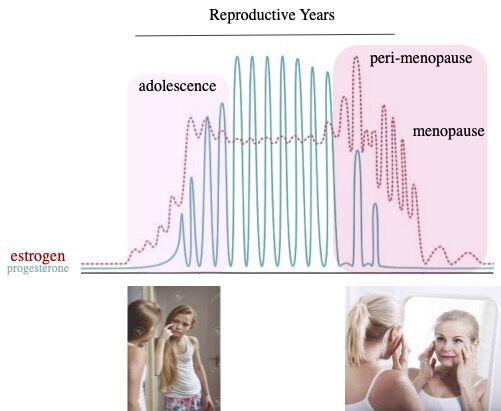
To explore this idea, it is interesting to consider that a woman’s brain is subject to natural oscillations in the levels of circulating ovarian hormones (estrogen and progesterone) throughout the reproductive years. These hormones fluctuate in synchrony with the menstrual cycle, with a direct impact on brain functions such as memory and emotions. Many important brain areas express the target receptor for the estrogen hormone and are thus highly attuned to changes in estrogen levels.
Yet both the beginning as well as the end of a woman’s reproductive years, namely adolescence and menopause, are times of much more extensive hormonal shifts. How these changes in hormone levels specifically impact the aging brain is now an area of strong scientific interest. Studies show that changes in estrogen can directly alter the properties of neurons in areas of memory formation. Studies in female mice show that estrogen loss can also negatively impact the survival of neurons in various brain areas and may set the stage for Alzheimer’s-like degeneration.
Old age is often a period of great wisdom, yet with Alzheimer’s, this is tragically lost amid devastating mental decline. As we seek the development of much-needed treatments for this disease, it is vital to also consider alternative strategies. Whether estrogen replacement therapy (ERT) can offset some of the risks of Alzheimer’s disease is not yet clear. Clinical findings suggest that ERT may be of greater benefit before a certain threshold of neural damage occurs. In some women, this may start as early as perimenopause, a transition period when the ovaries begin to lower estrogen production. This early phase of the hormone transition may turn out to be an important window of opportunity for reducing disease risk in aging women.
References
Conley AC, Albert KM, McDonald BC, Saykin AJ, Dumas JA, Newhouse PA. Estradiol treatment in young postmenopausal women with self-reported cognitive complaints: Effects on cholinergic-mediated cognitive performance. Hum Psychopharmacol. 2022 Feb 24;e2838. doi: 10.1002/hup.2838.
Cui J, Ait-Ghezala G, Sambamurti K, Gao F, Shen Y, Li R. Sex-Specific Regulation of β-Secretase: A Novel Estrogen Response Element (ERE)-Dependent Mechanism in Alzheimer's Disease. J Neurosci. 2022, 42(6):1154-1165.
Kight K, McCarthy MM. Androgens and the developing hippocampus. Biol Sex Differ. 2020, 11(1):30.
Lejri I, Grimm A, Eckert A. Mitochondria, Estrogen and Female Brain Aging. Front Aging Neurosci. 2018, 10:124.


