Mania
Antidepressant-Induced Mania Tied to Mitochondrial Activity
Increase in mitochondrial energetics is linked to treatment-emergent mania.
Posted May 2, 2023 Reviewed by Ekua Hagan
Key points
- Treatment-emergent mania is twice as common in patients taking antidepressants that increase, instead of decrease, mitochondrial activity.
- Categorization of antidepressants based on mitochondrial energetics has clinical value.
- These findings add to mounting evidence pointing to the involvement of mitochondrial dysfunction in the etiology of bipolar disorder.
When I was diagnosed with bipolar I disorder, I was in the midst of a severe manic episode with psychotic features. I was rail-thin and exercising fanatically—even in the middle of the night at a 24-hour gym. I slept as little as 15 minutes a night, and when I did sleep, I would wake up with my clothes and bed drenched in sweat. I experienced delusions of grandeur and hyper-religiosity, as well as heightened senses and creativity, among other classic symptoms of mania.
In retrospect, I had experienced manic and hypomanic episodes before—I just didn't realize it at the time. For almost 20 years, my bipolar disorder had been misdiagnosed and I had been treated for major depressive disorder and anxiety, for which I had tried a variety of different combinations of medicines. When that severe manic episode took hold, I had been taking the antidepressants Wellbutrin (bupropion) and Pristiq (desvenlafaxine). For individuals with bipolar disorder, those drugs are each known to induce mania on their own—and I took them together. Add in stressors such as an ugly divorce, estrangement from my daughters, and recovery from alcohol abuse, and it seemed like all roads were leading me to mania.
But why are some antidepressants associated with inducing mania but not others? A new study by a team of researchers led by Manuel Gardea-Resendez, M.D., of the Mayo Clinic provides some intriguing answers.
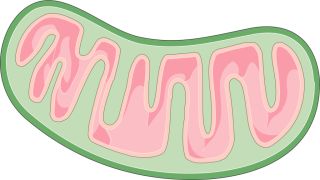
Bipolar Disorder and the Powerhouse of the Cell
Over the past 20 years, mounting evidence has pointed to the involvement of mitochondrial dysfunction in the etiology of bipolar disorder. The classic role for mitochondria is to generate energy through a process called oxidative phosphorylation, which relies in part on a set of electron transport chain (ETC) proteins. Reduced expression of mitochondrial ETC genes has been consistently found in the frontal cortex and hippocampus of patients with bipolar disorder, and impaired mitochondrial function has been implicated in various aspects of bipolar disorder, including risk for shifting into mania and/or psychosis.
Some antidepressants have been shown to increase ETC activity while others have been shown to decrease ETC activity. This led researchers to assess whether antidepressants that increase mitochondrial activity are associated with higher rates of antidepressant-induced mania (also called treatment-emergent mania). Study participants were chosen based on their history of antidepressant exposure and availability of clinical outcome measures.
After adjusting for age, sex, and subtype of bipolar disorder, researchers found that treatment-emergent mania was more than twice as common in patients exposed to antidepressants that increase mitochondrial energetics compared to participants exposed to antidepressants that decrease mitochondrial activity.
In addition, their findings suggest that the categorization of antidepressants based on mitochondrial energetics has clinical value, as compared to conventional categorization based solely on monoaminergic mechanism of action (e.g., selective serotonin reuptake inhibitors (SSRIs), serotonin norepinephrine reuptake inhibitors (SNRIs), norepinephrine dopamine reuptake inhibitors (NDRIs), and tricyclic antidepressants (TCAs)). Specifically, paroxetine (SSRI), nortriptyline (TCA), bupropion (NDRI), venlafaxine (SNRI), and imipramine (TCA) were found to increase mitochondrial ETC activity, compared to amitriptyline (TCA) and escitalopram (SSRI), which decreased mitochondrial ETC activity.
Conclusion
Results from this study provide support for the idea that amplified mitochondrial energetics in response to select antidepressants drives, at least in part, the pathophysiology of treatment-emergent mania. As stated by Gardea-Resendez, "Future clinical studies should investigate potential interactions between mitochondrial mechanisms of disease risk that may predispose to antidepressant associated treatment-emergent mania and may have a clear impact on the management and treatment of patients with bipolar disorder."
References
Gardea-Resendez, M., Coombes, B.J., Veldic, M. et al. Antidepressants that increase mitochondrial energetics may elevate risk of treatment-emergent mania. Mol. Psychiatry 28, 1020–1026 (2023). https://doi.org/10.1038/s41380-022-01888-x


