Suicide
You Can Prevent Suicide in Someone Close to You
How you, as in individual, can save valuable lives.
Posted August 1, 2020 Reviewed by Gary Drevitch
With 45,000 suicide deaths in the U.S. in 2016,1 someone has to do something.
I’m proposing that someone is you.
Sound outlandish? Maybe so, but would you respond similarly if I recommended that you learn to conduct cardiopulmonary resuscitation (CPR) for patients with cardiac arrest or the Heimlich maneuver for patients choking to death on a large bite of food? Those are more familiar topics, simply part of good emergency treatment for severe physical disorders.
So, let’s expand our horizon to include a mental health emergency demanding equally urgent attention: the suicidal person.
Just as everyone needs to be skilled in physical disease emergencies, so, in my opinion, should we all be skilled in identifying suicidal thoughts in others—and ensuring they receive immediate professional attention. After all, your skills handling suicidal emergencies most likely will involve people who are close to you. Valuable lives can be saved—and prevent the inordinate suffering that befalls loved ones left behind.
So, let’s see what this entails if you are interested.
Here are some high-risk situations where suicides are more likely to occur, although most people in these categories are not suicidal, and a minority of suicidal patients are not in any of them but in an overwhelming situation personally.2
- Depression and other mental disorders, including substance abuse
- Chronic physical disease, especially when disabling and when associated with chronic pain
- Prior suicide attempt or a family history of suicide, mental disorder, or substance abuse
- Past or present history of abuse, especially chronic
- Firearms in the home
- Recently released from prison or jail
- Exposure to suicides, including those of prominently celebrities as well as those close to the person.
And here are some direct clues that should make you suspicious that your friend or family member might be suicidal and require further questioning.2 Please realize, though, that all people who commit suicide do not exhibit these clues. In all instances, we have to talk with the person to find out, as I’ll describe shortly.
- Talking about wanting to die or feeling hopeless with no reason to live
- Talking more often about death
- Making a plan or exploring a way to kill themselves, perhaps looking online, stocking sleeping pills, or buying a gun
- Obsessing about how guilty and ashamed they feel
- Complaining of feeling trapped with no escape or solution
- Experiencing unbearable emotional or physical pain
- Talking about being a burden to others
- Withdrawing from family and friends
- Acting anxious or agitated
- Using more alcohol and/or drugs
- Changes in eating and sleeping habits
- Mood swings from very sad to very happy or even calm
- Becoming rageful and speaking of revenge
- Taking unusual risks, such as speeding
- Giving away important possessions and/or putting affairs in order, such as drawing up a will
- Saying goodbye to friends and family.
Now we’re coming to the difficult part: what you actually will do. To begin, the old adage that asking about suicide puts the thought into a person’s mind is not correct. It’s perfectly okay and safe to ask. Well, then, exactly how do we conduct this conversation?2
To begin, you establish a caring relationship, letting the person know you are interested in their well-being, perhaps having a 1-2 minute conversation about how things are going, listening for the above clues.3 It’s perfectly appropriate to ask about their feelings or emotions, indeed, I recommend this, simply ask directly with something like, “What’s the feeling that goes with that lost job (divorce; cancer diagnosis; death in the family; having no dates; flunking a test)?” It’s important to hear this out for a minute or two until you have a pretty good understanding of the situation. Then you address what we call the empathic skills to the emotion you have discovered, for example, that the person is upset or worried or angry or depressed. Unfortunately, while everyone tells us we should “be empathic,” no one tells us how! Here’s how. I coined a mnemonic to help remember these empathic skills.3,4 We NURS the emotion by:
- Naming it (“…so you’re pretty angry [worried, depressed, upset, stressed]…”)
- Understanding it (“…makes sense to me, I understand…”)
- Respecting it (“…thanks for telling me, you’ve had a tough time…”)
- Supporting it (“…let me know how I can help…”).
Of course our minds seek to complete the word suggested by NURS; add the letter ‘E” to make the word “nurse.” The ‘E’ stands for empathy—and can you think of anyone more empathic than our nurses, especially in the coronavirus pandemic. After actively understanding the problem and NURSing the patient’s emotion a few times, we are ready to directly inquire about suicidal intent.
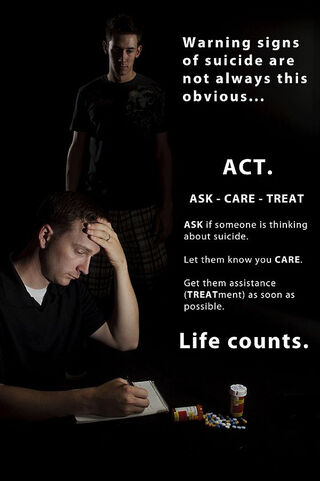
You ask two questions.
First, continuing in a supportive way, ask directly, for example, saying something like, “I’m concerned about you, that’s a lot to go through. Some people might have thoughts of death with all you’re dealing with, perhaps that life isn’t worth living or hoping just not to wake up in the morning. Have you had these thoughts?” Having thoughts of death does not mean someone is suicidal, but it’s serious business, adding further to the suspicion prompting you to inquire. If there have been no thoughts about death, you need go no further, just continue being supportive around whatever problem occasioned the conversation. On the other hand, if they have these thoughts, you now determine if the distressed person is actually suicidal.
Second, inquire about specific thoughts of suicide or self-harm, perhaps saying, “Sometimes people with those thoughts about death you mentioned think of taking their own life, have you ever thought about taking your life (or harming yourself)?” The answer (and how it’s given) is critical. “No, I don’t want to go to hell,” one person might respond emphatically; another might say, “Absolutely not, who’d take care of my cat?” If you get a convincing negative answer, nothing further is needed except, as above, to be supportive around their problem. But, if you do not get a clear rejection of the idea of suicide, for example, the person hedging, or if they say they have thought about taking their life, you have a four-alarm emergency.
Providing continued supportive comments, you now must ensure that they receive immediate help, the problem all the more serious if you learn they have a specific plan for killing or harming themselves (a collection of pills, a gun, tubing to connect to a car exhaust—remove them if possible). Don’t just advise the person to get help, take them to their doctor or the nearest emergency room. If they refuse, call 911. In any event, do not let them out of sight until under care. This is how these valuable lives can be saved.
I understand how difficult and scary this can be, it’s always tension-laden to ask about suicidal intention, especially when you identify it. My goal here is to provide you with the tools and motivation to save these lives. Try it. If you take the risk, you will save a life, often someone close to you.
Here’s a tip to make this easier. Imagine a scenario in which a person, perhaps someone you know, has suicidal intent. Practice (rehearse) the statements above in your own mind or out loud or with someone else. It helps to first have this experience verbalizing what you’ll say before you get into the stress of an actual interaction.
If more of us become comfortable using these skills, the public’s expertise in addressing suicidality can match the number of lives saved by cardiopulmonary resuscitation and the Heimlich maneuver.
Preventing suicide is a public health issue with nearly 50,000 lives yearly at stake. If we all pitch in and become alert to possible suicidal intent in those close to us, we can stem this tide.
References
1. Suicide rising across the US--More than a mental health concern. Centers for Disease Control and Prevention, 2018. (Accessed June 9, 2018, at https://www.cdc.gov/vitalsigns/suicide/index.html.)
2. Smith R, D'Mello D, Osborn G, Freilich L, Dwamena F, Laird-Fick H. Essentials of Pschiatry in Primary Care: Behavioral Health in the Medical Setting. New York: McGraw Hill, Inc; 2019
3. Fortin VI AH, Dwamena F, Frankel R, Lepisto B, Smith R. Smith's Patient-Centered Interviewing -- An Evidence-Based Method. 4th ed. New York: McGraw-Hill, Lange Series; 2019.
4. Smith RC, Hoppe RB. The patient's story: integrating the patient- and physician-centered approaches to interviewing. Ann Intern Med 1991;115:470-7.




