Hormones
Menopause and Hormone Replacement Therapy: A Woman's Dilemma
Treatment must be individualized, and a woman should have a thorough workup.
Posted February 15, 2022 Reviewed by Michelle Quirk
Key points
- Hormone replacement therapy for women around menopause has had a checkered past, with reports of increased cancer risks dating back to the 1930s.
- Therapy may be beneficial for hot flashes and night sweats, prevention of osteoporosis, and genitourinary symptoms, but it doesn't prevent aging.
- Most clinicians no longer believe "estrogen forever" and may prescribe the lowest dose for the shortest time within 10 years of menopause.

During the transition to menopause and even well beyond menopause for some, up to 75 percent of women will experience “bothersome symptoms,” including hot flashes and night sweats (Zhang et al., 2021).
“Bothersome” hardly captures the experience for many women. “A hot flash is a misnomer…it sounds like a flicker, short and quick, no big deal. But it’s more like an abdominal furnace on full blast creating a suffocating swelter” (Epstein, Aroused, 2018).
Hot flashes and night sweats, though hardly exclusive to menopause, are the most characteristic symptoms due to a decrease in estrogen and the ones for which women most commonly seek relief. Menopause, as a “social, cultural, and physiological transition,” though, has changed over time with more than 100 symptoms, including insanity, once attributed to it (Houck, 2002). For the many symptoms, including serious potential metabolic consequences of the menopause transition, see my post, The Turmoil of Menopause.
Depending on the symptoms, physicians developed “crude organotherapies” (Houck). Researchers did not isolate estrogen until 1929 (Houck) but realized that a substance in the ovaries was responsible for some symptoms.
Initially, estrogen replacement came from pregnant women in what was called “socialized estrogenicity” (i.e., an estrogen-rich woman gives to an estrogen-poor woman; Wilson and Wilson, 1972). By 1910, researchers turned to ground-up ovaries from farm animals (Wilson and Wilson; Fugh-Berman, 2015).

In the early 1940s, the US Food and Drug Administration (FDA) approved an estrogen extract, synthesized from pregnant mares (Houck). The name Premarin, the first conjugated estrogen, refers to its origin, pregnant mare’s urine (Fugh-Berman, 2015).
Early Concerns About Cancer
Concerns about the possible connection to cancer, though, had first arisen in the 1930s. In the 1940s, there were reports that both synthetic and natural estrogens were linked to cancer in animals (Houck). By the 1970s, researchers began to demonstrate a significant connection between estrogen replacement and endometrial cancer, causing some clinicians to urge caution (Berger and Fowler, 1977) about its “promiscuous” and “indiscriminate” use (Houck). They called for less "therapeutic enthusiasm and passion" and "more facts" (Graber and Barber, 1975).
No one was more enthusiastic about estrogen replacement than gynecologist Robert Wilson, whose 1966 book Feminine Forever sold millions of copies. Wilson and his wife, a nurse, wrote, "...a woman may have to spend half her life with dying or dead gonads.” With estrogen replacement, they continued, “Breasts and genital organs will not shrivel. Such women will be much more pleasant to live with and will not become dull and unattractive” (Wilson and Wilson).
What few people appreciated then was that Wilson had what we now call a major “conflict of interest” (Houck): His own foundation received substantial funding from three drug companies that manufactured hormone replacements (Fugh-Berman, 2015). In effect, Wilson's book “was sold as an expert’s advice but it was really one large advertisement” (Epstein).
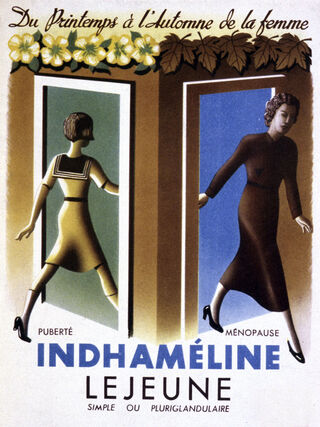
Despite concerns about possible links to cancer, many physicians and their patients thought of menopause as a deficiency disease, an “endocrinopathy,” requiring treatment (Fugh-Berman, 2015); hormone replacement, a term that entered the language by the mid-1960s (Oxford English Dictionary) became the prescription for ovarian failure (Houck).
Women's Health Initiative Study
Replacement therapy continued to have a checkered past and generate concern, despite efforts by the pharmaceutical companies to push for its use. Most notably was the National Institutes of Health–funded multicomponent Women's Health Initiative (WHI), a randomized study, initially involving more than 27,000 women (including 20 percent minorities) ages 50 to 79, to evaluate health benefits in postmenopausal women. Begun in the early 1990s, the hormone component of the trials evaluated estrogen alone or in combination with progesterone for coronary artery disease prevention, with breast cancer as a possible adverse effect (Prentice and Anderson, 2007). Researchers halted the trials several years earlier than anticipated when evidence accumulated that increased risks, including stroke, deep vein thrombosis, and breast cancer, outweighed benefits (Fugh-Berman et al., 2011).
When sales of the medications fell substantially, the pharmaceutical companies, with the assistance of physicians who had their own (often undeclared) conflicts of interest, doubled down their efforts to discredit the WHI study and claimed risks had been exaggerated (Fugh-Berman et al.). Ioannidis et al. found a significant contaminated "partisan stance" favoring hormone therapy in editorials, often with paragraphs "repeated verbatim" in the scientific literature (Tatsioni et al., 2010).
Hormone Replacement Today
Where do we stand now? Researchers have found that risks often depend on the dose, duration, route of administration (e.g., oral, transdermal, vaginal), and whether progesterone is added to estrogen. There is also a window of opportunity, the so-called timing hypothesis, where some clinicians believe it is safer to initiate replacement therapy within 10 years of menopause to avoid coronary heart disease (McNeill and Merriam, 2021; Prabakaran et al., 2022).
Hormone replacement now may be recommended for the vasomotor symptoms of hot flashes and night sweats, genitourinary symptoms (e.g., vaginal dryness and pain on intercourse), and prevention of osteoporosis (Pan et al., 2022; Vigneswaran and Hamoda, 2021). Symptom relief may also alleviate concomitant sleep difficulties as well as anxiety and depressed mood in some women (Vigneswaran and Hamoda).
Though not recommended as a “preventive strategy” specifically but rather as part of a more comprehensive approach to symptom relief (Stachowiak et al., 2015), some believe that estrogen replacement is beneficial for metabolic homeostasis: It can have a favorable effect on abdominal fat accumulation, lean body mass, and waist-to-hip ratio (Lovre et al., 2017). There are conflicting reports, sometimes related to differences in the population studied, on its effect on glucose levels and insulin sensitivity (DePaoli et al., 2021), and it does not alleviate hypertension (Lovre et al.). Further, its use cannot prevent aging (Maas, 2021).

Clinicians recommend an individualized approach (Kapoor et al., 2021), including an initial thorough workup for cardiovascular disease, the major killer of postmenopausal women, as well as a risk assessment for breast and endometrial cancer prior to initiating replacement therapy (Prabakaran et al.). They also recommend using the lowest dose for the shortest duration, usually fewer than five years (i.e., no "estrogen forever") (Pan et al., 2022).
There is some suggestion that a transdermal route is more likely to reduce the risk of venous thrombosis and stroke (Kapoor et al.; Maas). Combining estrogen with progesterone may reduce the risk of endometrial cancer, but may also increase the risk for breast cancer (Pan et al.). So-called custom-made "compounded" hormones are advertised "so that you'd think you are getting the free-range, grass-fed equivalent" but "buyer beware" as these fall out of the purview of the FDA (Epstein).
Considerable “uncertainty” still remains about the impact of hormone replacement on women’s health: Zhang et al. (2021), in a thorough literature review, found the quality of much of the research was “moderate to poor.” Unfortunately, the "precise association" of hormone therapy and the risk of cardiovascular diseases, thromboembolism, neurodegenerative diseases, breast cancer, and endometrial cancer "remains controversial" (Pan et al.).
References
Berger GS; Fowler WC Jr. (1977). Exogenous estrogens and endometrial carcinoma: review and comments for the clinician. Journal of Reproductive Medicine 18(4): 177-80.
De Paoli M; Zakharia A; Werstuck GH. (2021). The role of estrogen in insulin resistance: a review of clinical and preclinical data. American Journal of Pathology 191(9): 1490-1498.
Epstein RH (2018). Aroused: The history of hormones and how they control just about everything. New York: W.W, Norton & Company.
Fugh-Berman A. (2015). The science of marketing: how pharmaceutical companies manipulated medical discourse on menopause. Women’s Reproductive Health 2(1); 18-23.
Fugh-Berman et al (2011). Promotional tone in reviews of menopausal hormone therapy after the Women’s Health Initiative: an analysis of published articles. PLoS Medicine 8(3): e1000425.
Graber EA; Barber HR. (1975). The case for and against estrogen therapy. American Journal of Nursing 75(10): 1766-71; 1794.
Houck JA. (2002) How to treat a menopausal woman: a history, 1900-2000. Current Woman’s Health Reports 2: 349-355.
Kapoor E et al (2021). Menopausal hormone therapy in women with medical conditions. Best Practice & Research Clinical Endocrinology & Metabolism 35(6): 101578.
Lovre D; Lindsey SH; Mauvais-Jarvis F. (2017) Effect of menopausal hormone therapy on components of the metabolic syndrome. Therapeutic Advances in Cardiovascular Disease 11(1): 33-43.
Maas A H.E.M. (2021). Hormone therapy and cardiovascular disease: benefits and harms. Best Practice & Research Clinical Endocrinology & Metabolism 35(6): 101576.
McNeil MA; Merriam SB. (2021). Menopause. Annals of Internal Medicine 174(7): ITC97-ITC112.
Pan M et al (2022, Online ahead of print). Update on hormone therapy for the management of postmenopausal women. BioScience Trends P1-12.
Prabakaran S; Vitter S; Lundberg G. (2022) Cardiovascular disease in women update: ischemia, diagnostic testing and menopause hormone therapy. Endocrine Practice 28: 199-203.
Prentice RL; Anderson GL. (2007). The Women’s Health Initiative: lessons learned. The Annual Review of Public Health 29: 131-150.
Stachowiak G; Pertyñski T; Pertyñska-Marczewska. (2015) Metabolic disorders in menopause. Menopause Review 14(1): 59-64.
Tatsioni A; Siontis GCM; Ioannidis JPA. (2010). Partisan perspectives in the medical literature: a study of high frequency editorialists favoring hormone replacement therapy. Journal of General Internal Medicine 25(9): 914-919.
Vigneswaran K; Hamoda H. (2021). Hormone replacement therapy—current recommendations. Best Practice & Research Clinical Obstetrics and Gynecology. Dec 14; S1521-6934(21)00180-2.
Wilson RA; Wilson TA (1972). The basic philosophy of estrogen maintenance. Journal of the American Geriatrics Society XX(11): 521-523.
Zhang G-Q et al. (2021). Menopausal hormone therapy and women’s health: an umbrella review. PLoS Medicine 18(8): e100731.




