Health
How Psychologists Help Treat Polycystic Ovary Disease (PCOS)
How and why PCOS benefits from health behavior treatments.
Posted October 17, 2022 Reviewed by Ekua Hagan
Key points
- PCOS is the leading cause of female infertility and it is growing in prevalence.
- Although PCOS has multiple contributors, insulin dysregulation appears to be the most common and most important.
- Behavioral health treatments that address nutrition, sleep, and exercise can improve insulin function and help treat PCOS.
If you are a woman between the ages of 20 and 40, you have probably heard of polycystic ovary disease. In fact, women from this age group in the current generation are more likely than ever to be familiar with PCOS because the prevalence of PCOS has been steadily increasing (1). Since 1990, PCOS has quietly festered into a worldwide reproductive epidemic, becoming the leading cause of infertility among women as well as a frequent source of anxiety, shame, and depression.
Although most women with PCOS seek care exclusively from medical specialists in fields such as endocrinology and reproductive health, the underlying mechanisms of many, if not most, cases of PCOS are metabolic (2). Chief among the metabolic contributors to PCOS are hyperinsulinemia (excess insulin levels) and insulin resistance (impaired insulin response). Research suggests that two-thirds to three-fourths of women with PCOS demonstrate one or both of these insulin anomalies, including among women with normal body mass index (BMI) values (i.e., PCOS and co-occurring insulin dysfunction often affect women despite normal body weights). Because insulin dysfunction is frequently the root cause of PCOS, treatments that improve insulin function—including treatments from clinical health psychologists to improve behavioral health—should also be frontline treatments for PCOS.
Insulin and PCOS
How insulin dysfunction can cause a major reproductive health condition like PCOS isn't obvious. Most people, for instance, narrowly think of insulin as a hormone that controls blood glucose levels. While technically true (insulin levels rise during and after meals to keep blood glucose in a healthy range), the effects of insulin are far broader. Insulin, in fact, impacts the function of every organ in the body, including ovarian function in women. When insulin function goes array, therefore, ovarian function can become impaired. In the presence of hyperinsulinemia and insulin resistance, unfortunately, ovaries become compromised in their ability to convert circulating androgens (e.g., testosterone) into estrogens. This produces a buildup of androgen levels, amenorrhea, infertility, and numerous other unpleasant side effects. Although medicines can help with the physical and psychological symptoms of PCOS, reversing PCOS may require treatments that reduce hyperinsulinemia and improve insulin resistance (3). This is where a health psychologist can become a vital part of the woman's treatment team, irrespective of the mental health symptoms caused by her PCOS.
Nutrition and meal frequency
Health psychologists treat chronic medical diseases by helping people make positive changes in their nutrition, exercise, sleep, and stress management. Although improving the latter health habits can help prevent or treat many medical conditions, these behavioral interventions can directly assist women with PCOS because these interventions are highly effective specifically for reversing hyperinsulinemia and insulin resistance (4). That is, they address the core biological mechanisms causing PCOS.
Although many people think that improving nutrition means going on a diet, this is frequently incorrect. Particularly in the case of PCOS, the most helpful first steps towards improving nutrition come not from changing what the woman eats at all, but when and how often.
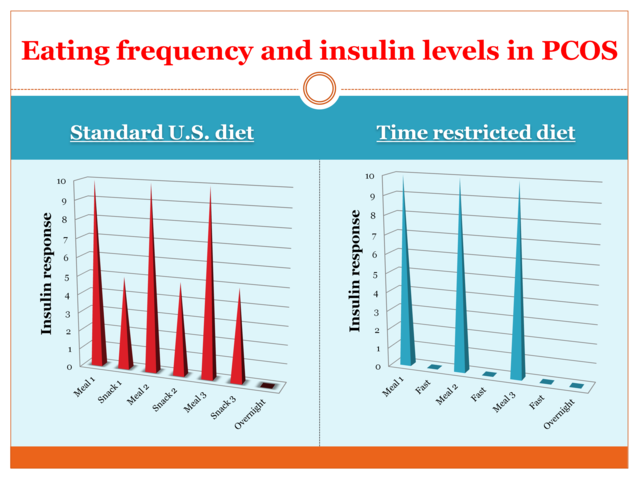
The figure below illustrates what happens to insulin levels when we follow a conventional U.S. diet—eating 3-4 meals plus snacks—versus a "time-restricted diet" where the same person eats only meals and only during an 8-12 hour window (e.g., from 8 a.m. to 6 p.m., with no food or caloric beverages consumed before or after the meals from that day). In the former case (left side of figure), insulin is elevated for approximately 16 hours a day—nearly every moment the person is awake. Because the person is constantly either eating or digesting food, insulin must remain elevated to control blood glucose levels. Over time, this pattern of eating leads to hyperinsulinemia and insulin resistance (3). In contrast, in the time-restricted eating plan shown on the right—even if the woman consumed the same types of foods—the less frequent meals and longer overnight fast allows insulin levels to return to baseline. Not surprisingly, the latter eating pattern has been shown to be highly beneficial for correcting the underlying mechanisms of PCOS (5).
Better sleep, better PCOS
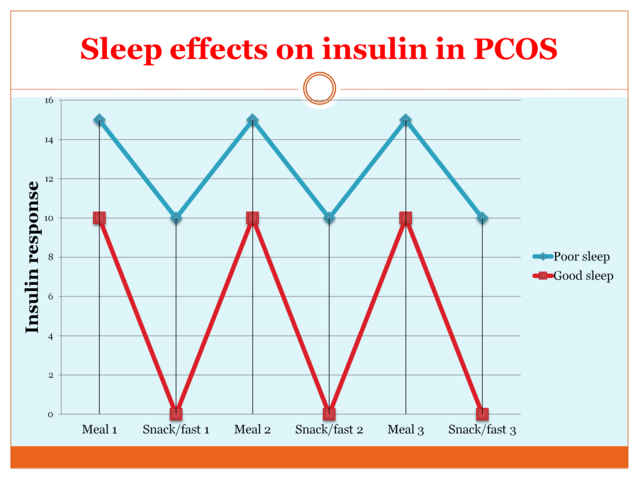
Poor sleep has rapid and severe effects on metabolic function, including the negative metabolic consequences of hyperinsulinemia and insulin resistance. Some laboratory studies (see figure below for an illustration), for example, indicate that poor sleep can produce a 50 percent or greater increase in insulin resistance within just a few days. In practice, this means that a woman with PCOS—despite following the same diet—would experience 50 percent higher blood glucose levels and insulin responses to her meals and snacks (the blue pattern in the figure below shows the frightening effect on insulin resulting from the combination of poor sleep and a U.S. diet. In contrast, the red pattern at the bottom indicates the strikingly improved profile resulting from a combination of a time-restricted eating plan and good sleep habits). Sadly, scientific reviews indicate that rates of sleep problems may be 50-100 percent higher among women with PCOS versus women without the condition. This combination of high prevalence and adverse impact on insulin parameters makes assessing and addressing sleep problems a critical component of PCOS treatment.
The good news is that common sleep problems such as insomnia and sleep apnea are highly treatable. Cognitive behavior therapy for insomnia (CBT-i), for example, is increasingly recognized as the gold standard treatment for insomnia, and the range of masks and treatment options for sleep apnea has never been larger or more effective. Recent studies examining the effects of treating sleep conditions such as insomnia and sleep apnea in women with PCOS are likewise very promising, indicating, for example, that regular CPAP use can improve insulin sensitivity by 40 percent (6).
Exercising for PCOS
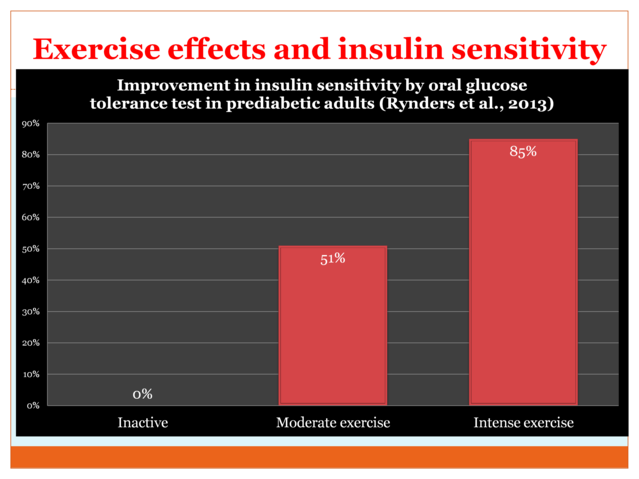
Sadly, when many women with PCOS are counseled about exercise, it is part of a generic recommendation for losing weight. This is unfortunate advice because regular exercise—regardless of exercise-related changes in weight—has rapid and potent benefits on insulin function. For example, the figure below summarizes improvements in insulin sensitivity among female and male adults with pre-diabetes (a condition—like PCOS—resulting from hyperinsulinemia and insulin resistance) from moderate and intense exercise. Measured using a controlled oral glucose tolerance test, participants in the moderate exercise condition showed a 51 percent improved response to glucose (indicative of greater insulin sensitivity). Even more impressive, those in the higher-intensity exercise condition showed an 85 percent improvement (7).
Importantly, the insulin benefits from exercise are realized within hours and days, long before any measurable changes on the scale occur. For this reason, not only should women with PCOS routinely receive encouragement and resources for exercise as part of their professional care, they should likewise receive information emphasizing that exercise is beneficial independent of weight loss. The latter information can potentially help exercise recommendations be better received by women with PCOS who may otherwise feel deterred by the twin stigmas of PCOS and weight loss.
Summary
Understanding the common metabolic causes of PCOS can be a game-changer for many women by opening up effective new behavioral treatment strategies. Although medical treatments remain the conventional care model for women with PCOS, the potent insulin effects of behavioral health interventions available from treatments provided by clinical health psychologists support a growing role for these specialists.
References
1. Motlagh Asghari, K., Nejadghaderi, S.A., Alizadeh, M. et al. Burden of polycystic ovary syndrome in the Middle East and North Africa region, 1990–2019. Sci Rep 12, 7039 (2022). https://doi.org/10.1038/s41598-022-11006-0
2. Marshall JC, Dunaif A. Should all women with PCOS be treated for insulin resistance? Fertil Steril. 2012 Jan;97(1):18-22. doi: 10.1016/j.fertnstert.2011.11.036.
4. Lim SS, Hutchison SK, Van Ryswyk E, Norman RJ, Teede HJ, Moran LJ. Lifestyle changes in women with polycystic ovary syndrome. Cochrane Database Syst Rev. 2019 Mar 28;3(3):CD007506. doi: 10.1002/14651858.CD007506.pub4.
5. Che X, Chen Z, Liu M, Mo Z. Dietary Interventions: A Promising Treatment for Polycystic Ovary Syndrome. Ann Nutr Metab. 2021;77(6):313-323. doi: 10.1159/000519302.
6. Tasali E, Chapotot F, Leproult R, Whitmore H, Ehrmann DA. Treatment of obstructive sleep apnea improves cardiometabolic function in young obese women with polycystic ovary syndrome. J Clin Endocrinol Metab. 2011 Feb;96(2):365-74. doi: 10.1210/jc.2010-1187.
7. Rynders CA, Weltman JY, Jiang B, Breton M, Patrie J, Barrett EJ, Weltman A. Effects of exercise intensity on postprandial improvement in glucose disposal and insulin sensitivity in prediabetic adults. J Clin Endocrinol Metab. 2014 Jan;99(1):220-8. doi: 10.1210/jc.2013-2687.




