PANDAS
The Intersection of Mental Health and the Immune System
Exploring new avenues of diagnosis and treatment in mental health care.
Posted February 28, 2024 Reviewed by Devon Frye
The current mental health crisis is showing no signs of abating. Suicide rates continue to rise, reaching the highest they have been in U.S. history.1 Chronic absenteeism has doubled in elementary students and is as high as 30 percent for high school students in the state I work in (Massachusetts).2
As a nation, we are racing to stem the crisis. We are talking about mental health more and demanding equity, access, and the de-stigmatization of those suffering. We also need innovative treatment discoveries, even cures.
In a 2013 Ted Talk, Dr. Thomas Insel, former director of the National Institute for Mental Health, described his belief that mental illness would see new medical advances imminently.3 Heart disease, stroke, and cancer deaths have plummeted after similar advances—yet suicide numbers have remained the same since 1950, and rates of disability from mental illness are the highest among any medical causes.4
Ten years later, we may finally have hope.

Ruling Out Medical Causes of Mental Illness
The unexpected silver lining of the pandemic is the knowledge that a virus can, and often does, cause psychiatric symptoms. A recent study published by the American Academy of Pediatrics reports that COVID-19 can impact children’s neurological and mental health.5 Up to 30 percent of people will experience neuropsychiatric symptoms post-COVID.6 Long COVID is linked to psychosis, depression, and encephalitis. 7
This isn’t just the “stress of the illness” causing mental health shifts. The virus creates changes in the brain and this knowledge—that the immune system impacts the brain—isn’t novel.
As early as 1905, syphilis was identified as causing rage, psychosis, and depression; when treated with antibiotics, these symptoms resolve.8 An older person presenting with sudden changes in behavior is routinely screened for urinary tract infection. A quick PubMed search of “infection-induced mental illness” between 2016 and 2024 shows 2,260 results
Any clinician who uses the DSM 5 to diagnose must be aware of these connections. In our differential diagnosis, we must “rule out medical” causes of mental health every time we diagnose.
As such, it is imperative we know about recent research findings (to ensure we are considering medical causes of mental health symptoms). These include:
- Group A Strep, and other infections/viruses, can cause acute onset of OCD and/or food restriction, known as PANS/PANDAS (Pediatric Acute Onset Neuropsychiatric Syndrome/Pediatric Autoimmune Neuropsychiatric Disorder Associated with Strep). 11
- Anti-NMDA encephalitis may present with symptoms of schizophrenia.12 (Suzannah Cahalan's book Brain on Fire details this well).
- Auto-immune conditions, such as lupus and celiac, are being tied to treatment-resistant mental illness. When the auto-immune illness is treated, the mental health symptoms recede.13
- Suicide is linked to neuroinflammation.9 Impacts to the body that trigger inflammation, such as COVID-19, may cause neuroinflammation, increasing the risk of suicide.10
Paradigm Shift: Both/And
When both of my children received PANS/PANDAS diagnosis, after years of treatment-resistant mental health issues, I assumed we would be trading our mental health support for medical. I viewed the DSM-5 medical rule-out as an either/or scenario. Our systems of care confirm this: Insurance bills separately, research is separate, providers are trained separately.
When both children began treatment with antibiotics and anti-inflammatories, I watched their OCD abate and their suicidality cease. I had never seen mental health heal in this way and I thought this medical intervention meant a cure.
But a cure, I learned, was only possible with both medical and mental health treatments. PANS/PANDAS, and immune-mediated conditions like it, require a both/and approach.
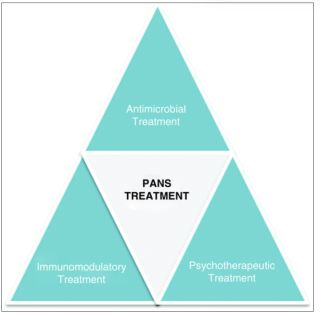
In the case of PANDAS, it is not the “stress” of having strep throat that causes the OCD and/or food restriction. That is caused by antibodies crossing the blood-brain barrier and attacking the basal ganglia.14 According to the PANS/PANDAS Physician Network (PPN) treatment guidelines, this is treated medically with antimicrobial and immunomodulatory treatments.15
The third arm of treatment, according to the PPN, is psychotherapeutic support, specifically cognitive behavioral therapy (CBT) and psychotropic medication.16 As the body heals, the brain also needs to heal. Our brains remember fear-based responses to protect us from danger. My children needed the support of mental health professionals to unlearn these responses and re-regulate their nervous systems.
Challenging the Status Quo
This felt revolutionary—and led me to conclude that instead of “ruling out” medical conditions, we should be ruling them in. The body could heal the brain and the brain could heal the body.
I started sharing this with family, friends, and at the school where I serve as Clinical Director. Caregivers who pursued diagnosis and treatment for this immune/brain health connection noted that their children, many of whom had treatment-resistant mental health issues, began to finally heal with the addition of medical interventions.
I excitedly shared with other professionals; how many more people could we help with this information? Medical, mental health, and educational professionals, however, often resisted or dismissed the question of medical “rule-outs” and the possible link to the immune system.
I understood. I too had initially dismissed the idea. I first heard about PANDAS six years before my youngest's diagnosis. Our then-pediatrician followed me into the lobby after a frantic sick visit for escalating OCD, separation anxiety, and mood lability. He whispered “Could this be PANDAS?” as I carried a hysterical 5-year-old out of the office.
I recall feeling confused and slightly offended by this idea. I considered myself an expert in mental health—my job was my vocation, I had a significant family history of mental illness, and I worked with countless children who presented as mine did. I felt sure I knew what was happening.
That doctor didn’t offer any new treatment or lab work and I didn’t explore it further, as if we made a pact that the status quo was safest. For the next six years, we both watched my child become sicker while we frantically tried every mental health treatment possible.
I heard of PANS/PANDAS again from another mother right at the time I thought we would lose them to suicide. None of the treatments I knew to be best practice were working. I was ready to try anything to save them.
My reaction, and the reaction of many of the professionals I have shared this information with, may be understood better as the Semmelweis Reflex. This is defined as “a primal human behavioral tendency to stick to preexisting beliefs and to reject fresh ideas that contradict those beliefs.”17
Dr. Semmelwies was a physician who, around the year 1847, pioneered the concept of handwashing before examining patients. His discovery that mortality rates dropped when doctors washed their hands between patients was initially ignored, dismissed, and ridiculed. The advent of germ theory in the 1860s substantiated Dr. Semmelwies’ theory and we have all been washing our hands ever since. 18
Who Are We Missing?
This pattern of resisting change has repeated itself throughout history, yet delayed diagnosis and treatment of these illnesses have devastating results. Through my advocacy, I have stories of countless families similar to ours and I work closely with two mothers whose children (Alex Manfull and Louisa Johnson) tragically, and completely unexpectedly, took their own lives as a result of these illnesses.
In Susannah Cahalan’s book, The Great Pretender, she describes the pain of realizing that while she was saved when her symptoms of schizophrenia were attributed to Anti-NMDA encephalitis, many others were left behind.19 Schizophrenia is one of the top 15 causes of disability worldwide and those diagnosed have an increased risk of premature death.20Schizophrenia is also known to be diagnosed significantly more among black individuals than their white counterparts.21
Equity and access for all means everyone should receive a rule out (rule in!) of medical cause each time a mental health diagnosis is given. Those of us who have watched loved ones heal because someone told us about these illnesses, consider ourselves the “lucky ones” who received a differential diagnosis.
We don’t have time to wait the 17 years it typically takes research to reach medical practice.22 We must all demand that these advances be incorporated into everyone's practice—to ensure our most vulnerable are not relegated to lifetimes of chronic mental illness, even suicide, when there may be hope for healing.
References
1. Curtin, S., Garnett, M.. and Ahmad, F. (2023, November). Provisional Estimates of Suicide by Demographic Characteristics: United States, 2022. The Center for Disease Control. https://www.cdc.gov/nchs/data/vsrr/vsrr034.pdf
2. Adame, Diane. (2023, November). Chronic absenteeism still high among Mass. students, new data shows. WGBH. https://www.wgbh.org/news/education-news/2023-11-21/chronic-absenteeism…
3. Insel,T. (2013, January). Toward a New Understanding of Mental Illness [Video]. TED Conferences. https://www.ted.com/talks/thomas_insel_toward_a_new_understanding_of_me…
4. Insel,T. (2013, January). Toward a New Understanding of Mental Illness [Video]. TED Conferences. https://www.ted.com/talks/thomas_insel_toward_a_new_understanding_of_me…
The figure outlines symptoms and conditions, grouped by body system, which have been associated with the PASC (Postacute sequelae of SARS CoV-2)
Source: Rao S, Gross RS, Mohandas S, et al. Postacute Sequelae of SARS-CoV-2 in Children. Pediatrics. 2024;153(3):e2023062570
5. Elmazny A, Magdy R, Hussein M, Elsebaie EH, Ali SH, Abdel Fattah AM, Hassan M, Yassin A, Mahfouz NA, Elsayed RM, Fathy W, Abdel-Hamid HM, Abdelbadie M, Soliman SH. Neuropsychiatric post-acute sequelae of COVID-19: prevalence, severity, and impact of vaccination. Eur Arch Psychiatry Clin Neurosci. 2023 Sep;273(6):1349-1358. doi: 10.1007/s00406-023-01557-2. Epub 2023 Jan 27. PMID: 36707454; PMCID: PMC9882743.
6. Elmazny A, Magdy R, Hussein M, Elsebaie EH, Ali SH, Abdel Fattah AM, Hassan M, Yassin A, Mahfouz NA, Elsayed RM, Fathy W, Abdel-Hamid HM, Abdelbadie M, Soliman SH. Neuropsychiatric post-acute sequelae of COVID-19: prevalence, severity, and impact of vaccination. Eur Arch Psychiatry Clin Neurosci. 2023 Sep;273(6):1349-1358. doi: 10.1007/s00406-023-01557-2. Epub 2023 Jan 27. PMID: 36707454; PMCID: PMC9882743.
7. Efstathiou V, Stefanou MI, Demetriou M, Siafakas N, Makris M, Tsivgoulis G, Zoumpourlis V, Kympouropoulos SP, Tsoporis JN, Spandidos DA, Smyrnis N, Rizos E. Long COVID and neuropsychiatric manifestations (Review). Exp Ther Med. 2022 May;23(5):363. doi: 10.3892/etm.2022.11290. Epub 2022 Apr 1. PMID: 35493431; PMCID: PMC9019760.
8. Harrington,A. (2019). Mindfixers. W.W.Norton & Company.
9. Wen-Jie Yan, Chun-Lei Jiang, Wen-Jun Su. Life in the flame: Inflammation sounds the alarm for suicide risk. Brain, Behavior, & Immunity - Health,
Volume 14,2021 100250,ISSN 2666-3546, https://doi.org/10.1016/j.bbih.2021.100250.
10. Costanza A, Amerio A, Aguglia A, Serafini G, Amore M, Hasler R, Ambrosetti J, Bondolfi G, Sampogna G, Berardelli I, Fiorillo A, Pompili M, Nguyen KD. Hyper/neuroinflammation in COVID-19 and suicide etiopathogenesis: Hypothesis for a nefarious collision? Neurosci Biobehav Rev. 2022 May;136:104606. doi: 10.1016/j.neubiorev.2022.104606. Epub 2022 Mar 12. PMID: 35289272; PMCID: PMC8916836.
11. PANDAS Physicians Network. (2024). Research. PANDAS Physicians Network. https://www.pandasppn.org/research-library/
12. Kayser MS, Dalmau J. Anti-NMDA receptor encephalitis, autoimmunity, and psychosis. Schizophr Res. 2016 Sep;176(1):36-40. doi: 10.1016/j.schres.2014.10.007. Epub 2014 Oct 25. PMID: 25458857; PMCID: PMC4409922.
13. Ravan JR, Chatterjee S, Singh P, Maikap D, Padhan P. Autoimmune Rheumatic Diseases Masquerading as Psychiatric Disorders: A Case Series. Mediterr J Rheumatol. 2021 Jun 30;32(2):164-167. doi: 10.31138/mjr.32.2.164. PMID: 34447914; PMCID: PMC8369283.
14. Platt MP, Agalliu D, Cutforth T. Hello from the Other Side: How Autoantibodies Circumvent the Blood-Brain Barrier in Autoimmune Encephalitis. Front Immunol. 2017 Apr 21;8:442. doi: 10.3389/fimmu.2017.00442. PMID: 28484451; PMCID: PMC5399040.
15. Pandas Physicians Network. (2024). Diagnostic Flowchart and Treatment Guidelines. Pandas Physicians Network.https://www.pandasppn.org/diagnose/
16. Pandas Physicians Network. (2024). Diagnostic Flowchart and Treatment Guidelines. Pandas Physicians Network.https://www.pandasppn.org/diagnose/
17. Gupta VK, Saini C, Oberoi M, Kalra G, Nasir MI. Semmelweis Reflex: An Age-Old Prejudice. World Neurosurg. 2020 Apr;136:e119-e125. doi: 10.1016/j.wneu.2019.12.012. Epub 2019 Dec 16. PMID: 31837492.
18. Gupta VK, Saini C, Oberoi M, Kalra G, Nasir MI. Semmelweis Reflex: An Age-Old Prejudice. World Neurosurg. 2020 Apr;136:e119-e125. doi: 10.1016/j.wneu.2019.12.012. Epub 2019 Dec 16. PMID: 31837492.
19. Cahalan, Susannah, (2020). The Great Pretender. Hachette Book Groups, Inc.
20. Accelerating Medical Partnerships. (2023, April). Schizophrenia. National Institutes for Health. https://www.nih.gov/research-training/accelerating-medicines-partnershi….
21. Faber SC, Khanna Roy A, Michaels TI, Williams MT. The weaponization of medicine: Early psychosis in the Black community and the need for racially informed mental healthcare. Front Psychiatry. 2023 Feb 9;14:1098292. doi: 10.3389/fpsyt.2023.1098292. PMID: 36846217; PMCID: PMC9947477.
22. Morris ZS, Wooding S, Grant J. The answer is 17 years, what is the question: understanding time lags in translational research. J R Soc Med. 2011 Dec;104(12):510-20. doi: 10.1258/jrsm.2011.110180. PMID: 22179294; PMCID: PMC3241518.


