Therapy
Narrative Therapy in Maternal Mental Health Care
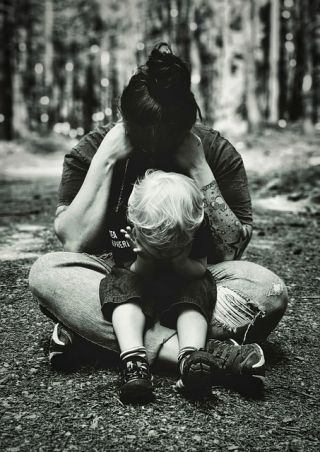
Sharing stories of perinatal struggle, with support, can accelerate healing.
Posted November 27, 2023 Reviewed by Jessica Schrader
Key points
- Perinatal mental health encompasses depression, anxiety, psychosis, PTSD, and more.
- Narrative therapy can help psychologically-struggling parents digest their experience and recover.
- Specialized training is available for therapists looking to work in perinatal mental health.

Pregnancy-related mental health is often more complicated than depression arising immediately after delivery. To scratch the surface, it's finally recognized that depression and other complications can develop anytime during pregnancy or after delivery; hence, the more accepted current term, peripartum or perinatal mental health.
Further, women can also experience perinatal mania, psychosis, symptoms of OCD, and other forms of anxiety. And what about those who can't conceive, a child does not survive the birth, or serious medical complications arise during delivery? There can be psychological trauma and grief. In addition, men can also struggle psychologically at this time.
Another mental health pandemic
To give an idea of the scope of perinatal mental health needs, consider these statistics from Blue Dot Project, a perinatal mental health website:
- In the U.S. alone, annually, 600,000-plus women suffer a maternal mental health need reaching disorder status.
- Upwards of 50% of pregnant women living in poverty encounter a pregnancy-related mental health problem.
- Less than 15% receive treatment.
In the past decade, researchers have paid more attention to what mothers have always known. That is, pregnancy-related mental health complications don't always exist in a vacuum that magically resolves after some adjustment. This is perhaps best summed up by Pawluski and Dickens (2019) who explained how peripartum mental health has suffered research neglect, especially antepartum, or pre-delivery, depression, and anxiety.
Such neuroses have shown unique neurobiological profiles, said the authors, suggesting the need for unique interventions for better outcomes. "Unfortunately, we know very little about how the brain changes during a healthy pregnancy, let alone in a diseased state," finished the authors.
Peripartum psychiatric complications not only affect the mother, but are associated with mother-child bonding complications, failure to thrive in extreme cases, and general domestic discord, ultimately affecting the children. Further, according to the Blue Dot Project (2023), 1 in 10 fathers also experience a significant perinatal mental health problem. Howard and Khalifeh (2020) provide a comprehensive review of all of these matters in their paper, Perinatal Mental Health: A Review of Progress and Challenges.
All of this, of course, begs the question if women are being adequately assessed and treated.
Perinatal mental health specialists
Jessica Petit, a Massachusetts-based mental health counselor, felt called to work in perinatal mental health. She historically used narrative therapy to work with psychologically traumatized patients. After learning about the lack of providers for maternal mental health, she changed her target population. Jessica underwent a year of training to be versed in maternal mental health needs, and merged it with her knack for narrative therapy. Things started coming full circle when, after the birth of her daughter, Jessica experienced significant postpartum depression. Then, in 2020, she miscarried a baby boy. "I was not well. I'd say I went off the deep end," she revealed.
Jessica's midwife eventually suggested that she contact a narrative therapist to digest her own grief and recultivate her well-being. "I was the one that did that work with others," she said, "I didn't want to do it, and avoided it." Eventually, she gave birth to a boy, but found herself riddled with affective difficulties. "I had a lot of grief and anger," she continued. "I was a nasty person. It wasn't good for me, my marriage, or parenting." Jessica revisited the idea of telling her story, and the results, she explained, were life-changing.
Drawing together her profession and her newfound empathy for traumatic birthing experiences, Jessica aimed to help mothers in similar situations discover, or even constructively grieve, a path forward, and decided to launch it in book form. She posted on Facebook mothering groups about her experience and asked if others were willing to share theirs. Jessica sought not only to encourage healing, but to provide a sense of community to mothers who were perhaps suffering alone, and encourage forward motion.
"The response was overwhelming," said Jessica. Most were unable to commit to the project, but the interest was there. Ultimately, 16 women contributed to Jessica's A Woman's Journey: Postpartum Healing (2023). The stories capture the experiences of women with peripartum depression, anxiety, psychosis, and PTSD, those with stillborn children, miscarriages, stresses of in vitro fertilization, and even postpartum struggles with substance abuse. All the proceeds of Jessica's book go to Empty Arms, a Western Massachusetts foundation that helps mothers/families who suffered a stillbirth or other perinatal tragedy.
The peripartum narrative process
Reflecting on her work with women struggling, Jessica relayed a powerful process. "When I was working with someone," she began, "I'd type along as they told me their story." At the end of the session, she would debrief with the patient and provide coping mechanisms if required after revisiting something so difficult. The previous session was reviewed at the start of each new session, and material could be added or changed based on what the woman thought about in between. Jessica likened this process to desensitization, each session allowing the woman to return to her experience a bit more and further digest and integrate it.
After the story was completed, Jessica would read it to her patient. "Yeah, someone knows their story, but when someone else reads it to them, it makes it more objective, it's a different experience," she said. After talking about that experience, the woman would then read the story aloud to Jessica. "This," said Jessica, "makes it personal in that they're conveying the experience out loud. It's no longer something internalized that they're lonely with. It's cathartic." After this reading, she has had women comment, "That happened?" opening a dialogue into a deeper healing process.
Becoming a peripartum therapist
Jessica shared that, despite the gaining interest in women's reproductive health, therapists for this niche remain lacking. A cursory internet search uncovers many therapists offering assistance with postpartum depression, but few with the other perinatal concerns she mentioned.
Jessica offered that, first, it's important to be aware of the fact that perinatal mental health is much more complicated than knowing how to work with depression. With that in mind, she finished with these two suggestions for those wishing to become a perinatal/reproductive health psychotherapist:
- Gain formal training in the topic: Jessica offered that she did her training through Postpartum Support International, and 2020 Mom (now known as Policy Center for Maternal Mental Health).
- Be aware of countertransference: Therapists often gravitate toward certain interests because of someone being touched by the matter. Thus, they can harbor ongoing conflicts and blind spots that could present treatment complications. For instance, someone who has been struggling to get pregnant, or whose partner is struggling, could harbor jealousy toward a patient who reaches success while in therapy. In turn, irritation toward them might surface, rendering it troublesome to maintain empathy and motivation to work intimately with them.
Disclaimer: The material provided in this post is for informational purposes only and is not intended to diagnose, treat, or prevent any illness in readers or people they know. The information should not replace personalized care or intervention from an individual’s provider or formal supervision if you’re a practitioner or student.
To find a therapist, please visit the Psychology Today Therapy Directory.
References
Pawluski, J. & Dickens, M. (2019). Pregnancy: A final frontier in mental health research. Archive of Women's Mental Health, 22(6): 831-832. doi: 10.1007/s00737-019-00988-y.
Petit, J. (2023). A woman's journey: Postpartum healing. Independently published.
The Blue Dot Project (2023). https://www.thebluedotproject.org/




